Diabetic Foot Ulcer Stages
If you have diabetes or poor circulation, you may risk developing foot ulcers. Foot ulcers are open sores or wounds that can occur anywhere on the foot, but are commonly found on the big toe, ball of the foot, and heel. Foot ulcers can be a serious complication of diabetes and, if left untreated, can lead to infection, gangrene, and even amputation.
This article will look closely at foot ulcers, their stages, and how they can be treated.
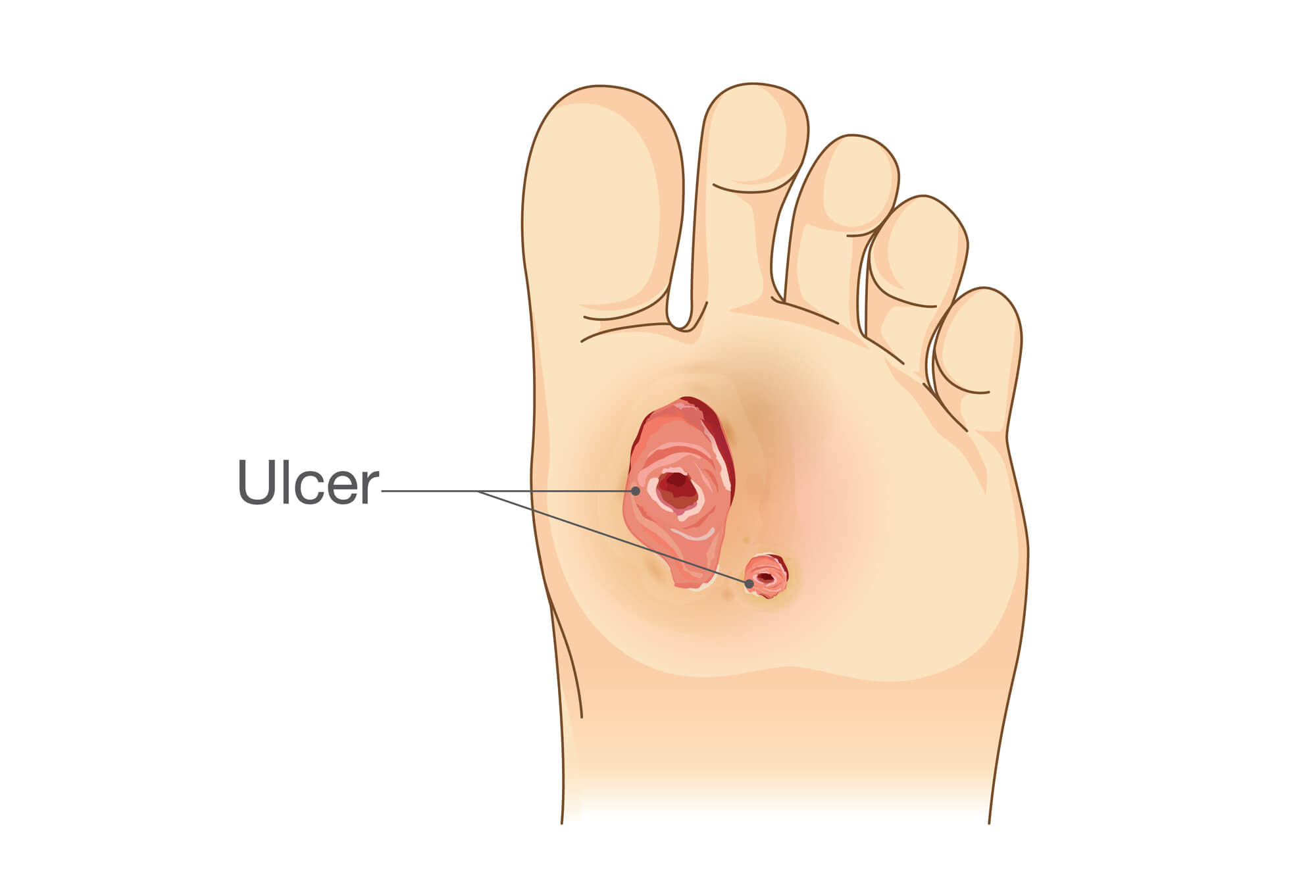
What is a Foot Ulcer?
A foot ulcer is an open sore or wound that can occur anywhere on the foot. Foot ulcers are a common complication of diabetes and can be caused by poor circulation, nerve damage, and high blood sugar levels. Ulcers can range in severity from a superficial blister to a deep wound penetrating the bone and tissue.
Stages of Foot Ulcers
Foot ulcers are categorized into four stages based on the depth and severity of the wound. Each stage has its own set of characteristics and requires different treatment options.
Stage 1: Redness and Swelling
The first stage of a foot ulcer is characterized by redness and swelling around the affected area. This stage may also include the development of a callus or corn, a sign of excessive pressure or friction on the foot. At this stage, the skin has not broken down yet, and there is no visible wound.
If detected early, stage 1 foot ulcers can often be treated with proper foot care and offloading to relieve pressure on the affected area. This may include wearing shoes with extra padding or using orthotics to redistribute pressure.
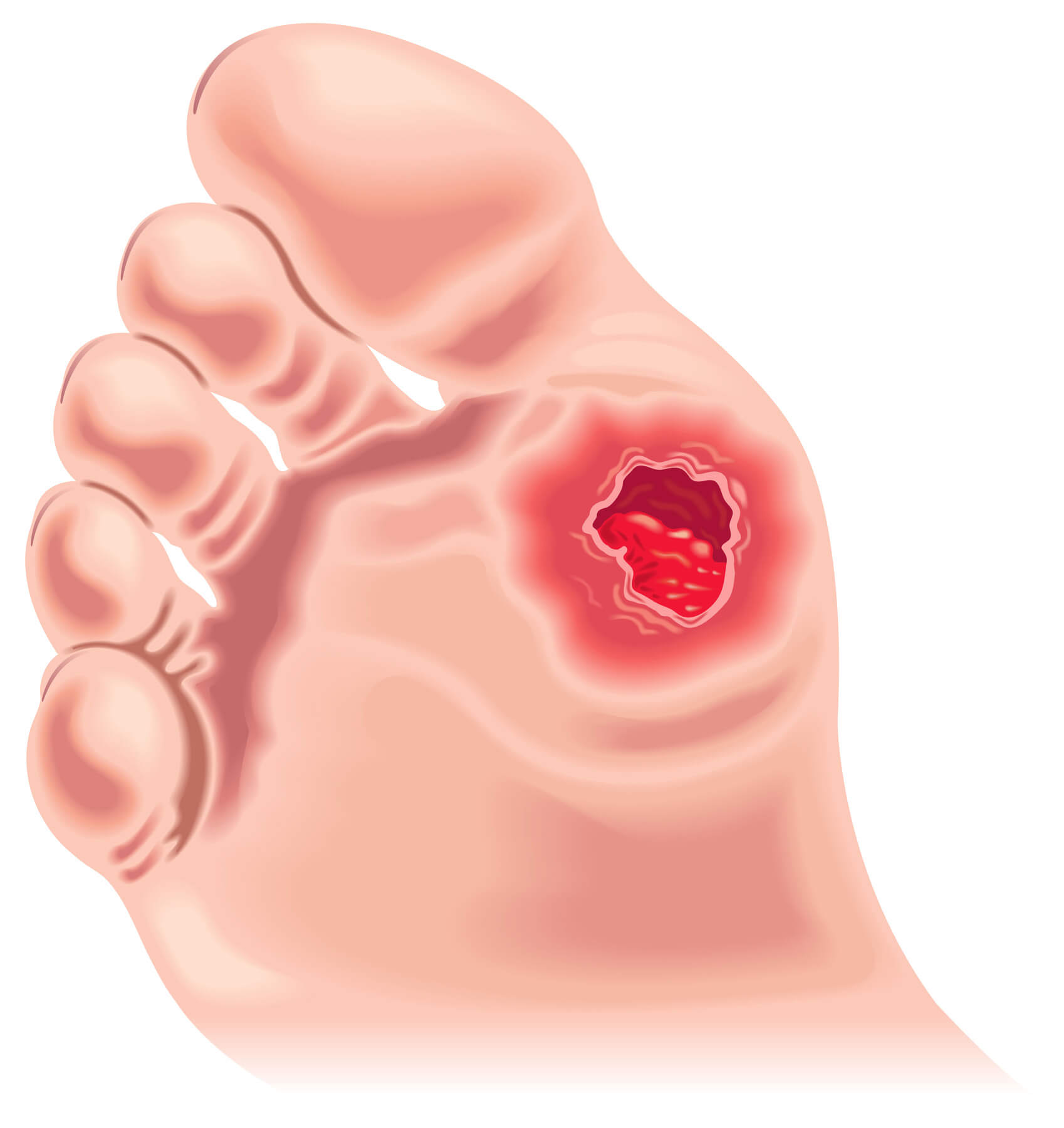
Stage 2: Blisters or Shallow Ulcers
The skin has broken down in stage 2 foot ulcers, and a blister or shallow ulcer has formed. This stage is often accompanied by drainage from the wound, and the area may appear swollen and red.
At this stage, seeking medical attention is important to prevent infection and promote healing. Treatment options may include wound care, offloading, antibiotics, or other medications to treat the infection.
Stage 3: Deep Ulcers with Visible Fat or Muscle Tissue
Stage 3 foot ulcers are deep wounds that extend into the fat or muscle tissue. The wound may be irregularly shaped, and there may be drainage and a foul odor. The affected area may appear swollen and red, and there may be a visible blood vessel or bone.
At this stage, treatment is more complex and may include more aggressive wound care, such as debridement (removing dead tissue), and possibly surgery to remove infected or necrotic (dead) tissue. Offloading is also important to prevent further tissue damage.
Stage 4: Bone and/or Joint Involvement
The most severe stage of foot ulcers is stage 4, which involves bone and/or joint involvement. The wound may be very deep, exposing bone, tendon or ligament damage, and there may be signs of osteomyelitis (infection of the bone) or sepsis (infection of the blood).
At this stage, immediate medical attention is necessary to prevent further complications and potentially life-threatening infections. Treatment may involve surgical intervention, such as amputation or realignment of bones and tendons, aggressive wound care and offloading.
Treatment of Foot Ulcers
The treatment of ulcers depends on the stage and severity of the wound. Treatment options may include:
Wound Care
Proper wound care is essential for the healing of foot ulcers. This may include cleaning the wound, removing dead tissue (debridement), and dressing the wound with appropriate materials. Wound dressings may vary depending on the ulcer stage and may include hydrogels, foams, and antimicrobial dressings. Keeping the wound clean and dry is important to prevent infection and promote healing.
Offloading
Offloading, or taking pressure off the affected area, is an important part of ulcer treatment. This may involve using a special boot or cast or using crutches or a wheelchair to avoid putting weight on the foot. Proper offloading can help prevent further tissue damage and promote healing.
Medications
Medications may be used to treat infection, relieve pain, and improve blood flow to the affected area. Antibiotics or other medications may be prescribed to prevent or treat the infection. Pain relief medication may be prescribed to manage pain. Blood sugar control is also important to promote the healing of ulcers in individuals with diabetes.
Surgery
In severe cases, surgery may be necessary to remove dead tissue or to realign bones and tendons. Surgical intervention may also be necessary in cases of deep infection or osteomyelitis. Amputation may be necessary if there is extensive tissue damage or if the wound does not heal despite all other treatment options.
Lifestyle Changes
Lifestyle changes may also be recommended to help promote healing and prevent further foot ulcers. This may include quitting smoking, managing diabetes, maintaining a healthy diet and exercise plan, and improving foot care practices.
Prevention of Diabetic Foot Ulcers
Preventing foot ulcers is essential for individuals with diabetes or poor circulation. Here are some tips for preventing ulcers:
Foot Care
Proper foot care is essential for preventing foot ulcers. This may include washing your feet daily with warm water and mild soap and drying them thoroughly. It is also important to check your feet daily for any signs of injury or redness, especially if you have decreased sensation in your feet. Additionally, trim your toenails straight across and avoid cutting corners to prevent ingrown nails.
Footwear
Wearing properly fitting shoes and socks is also important in preventing foot ulcers. Proper footwear can help prevent friction and pressure on your feet, leading to blisters and sores. Avoid walking barefoot or wearing shoes without socks. If you have foot deformities or other foot problems, your podiatrist may recommend special shoes or inserts to help redistribute pressure and prevent ulcers.
Lifestyle Changes
Lifestyle changes may also be recommended to help prevent ulcers. Avoid smoking and limit alcohol consumption, which can contribute to poor circulation. It is also important to maintain healthy blood sugar levels if you have diabetes, as high blood sugar can damage nerves and blood vessels in the feet.
Regular Foot Exams
Regular foot exams with a podiatrist or foot and ankle specialist are important for preventing foot ulcers. Your healthcare provider can help identify any foot problems early and provide appropriate treatment to prevent complications. If you have diabetes or poor circulation, scheduling a foot exam at least once a year or more frequently if you have any foot problems is recommended.
Blood Flow
Maintaining healthy blood flow to the feet is also important in preventing foot ulcers. This may include regular exercise to improve circulation, such as walking, cycling, or swimming. Wearing compression stockings or other compression garments may also help improve foot blood flow.
If you have diabetes or poor circulation, scheduling regular foot exams with a podiatrist or foot and ankle specialist is important. Your healthcare provider can help you identify any foot problems early and provide appropriate treatment to prevent complications.
Conclusion
Foot ulcers are a common complication of diabetes and poor circulation, but they can be prevented and managed with proper foot care and treatment. Recognizing the stages of foot ulcers and seeking medical attention early can help prevent complications and improve healing. If you suspect an ulcer, consult a podiatrist or foot and ankle specialist immediately for proper diagnosis and treatment.

