Tendinopathy vs. Tendonitis
Tendon conditions, such as tendinopathy and tendonitis, can cause pain and limit mobility. This article aims to differentiate between tendinopathy and tendonitis, provide insights into their causes and symptoms, and explore various treatment options available.
Understanding Tendinopathy
Tendinopathy is a broad term encompassing various tendon disorders characterized by degeneration rather than inflammation. Two common types of tendinopathy are tendinosis and paratenonitis. Tendinosis refers to the degenerative changes within the tendon itself, while paratenonitis involves inflammation of the paratenon, the protective sheath surrounding the tendon. These conditions often develop due to repetitive overuse, aging, poor biomechanics, or inadequate healing of a previous injury.
Understanding Tendonitis
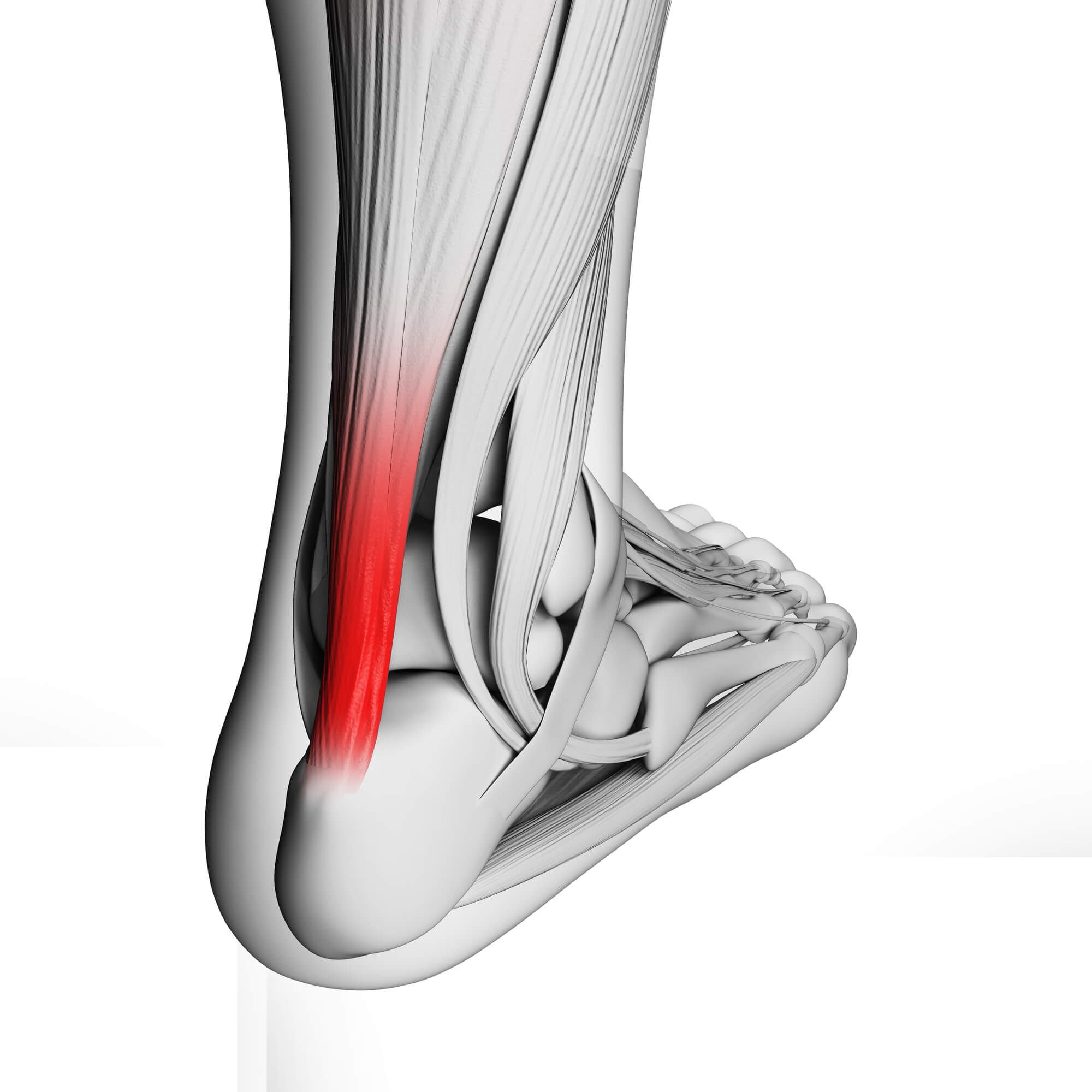
Tendonitis, on the other hand, refers to inflammation of the tendon. It typically occurs as a result of repetitive strain or acute trauma. Common examples include Achilles tendonitis, tennis elbow (lateral epicondylitis), and golfer's elbow (medial epicondylitis). Tendonitis is associated with localized pain, tenderness, and swelling, often exacerbated by activity.
The Differences Between Tendinopathy and Tendonitis
Tendinopathy and tendonitis differ in their underlying pathophysiology. While tendonitis is primarily an inflammatory condition, tendinopathy involves degenerative changes within the tendon structure, including collagen breakdown, increased vascularity, and abnormal healing response. A lack of significant inflammation often characterizes tendinopathy, but it can still result in pain, stiffness, and functional limitations.
Symptoms of Tendinopathy and Tendonitis
The symptoms of tendinopathy and tendonitis can overlap but also have distinct characteristics. Both conditions are typically present with localized pain, tenderness, and stiffness. However, tendonitis tends to cause more acute pain during or immediately after activity, while tendinopathy may involve chronic pain that worsens over time. In severe cases, tendon rupture can occur, leading to sudden weakness and loss of function.
Diagnosis of Tendinopathy and Tendonitis
Accurate diagnosis is crucial for effective treatment. A podiatrist or sports medicine specialist will conduct a comprehensive examination, including a detailed medical history and physical assessment. Diagnostic imaging, such as ultrasound or MRI scans, may be utilized to assess the extent of tendon damage. These evaluations help differentiate between tendinopathy and tendonitis and guide appropriate treatment strategies.
Treatment Options for Tendinopathy and Tendonitis
Non-Surgical Treatment
Non-surgical approaches are usually the initial line of treatment. They include:
- Rest, Ice, Compression, and Elevation (RICE): Resting the affected area, applying ice packs, compression, and elevating the limb can help reduce pain and swelling.
- Physical Therapy: Targeted exercises and stretching can promote tendon healing, strengthen the surrounding muscles, and improve the range of motion.
- Orthotic Devices and Footwear Modifications: Orthotic inserts or braces can support and offload the affected tendon and correct biomechanical abnormalities.
Medical Interventions
In some cases, medical interventions may be necessary. These may include:
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) or other pain relievers can help manage pain and reduce inflammation.
- Corticosteroid Injections: These injections deliver anti-inflammatory medication directly into the affected tendon, providing localized relief.
- Platelet-Rich Plasma (PRP) Therapy: PRP therapy involves injecting concentrated platelets from the patient's blood into the tendon, stimulating the body's natural healing response and promoting tissue regeneration.
Surgical Intervention (if applicable)
Surgery is typically considered when conservative treatments fail to provide relief or in cases of severe tendon damage. Surgical options may include tendon debridement (removing damaged tissue), tendon repair, or, in rare cases, tendon reconstruction using grafts.
Rehabilitation and Recovery
After treatment, rehabilitation plays a vital role in restoring function and preventing recurrence. Physical therapy exercises are essential for strengthening the tendon, improving flexibility, and enhancing overall musculoskeletal health. Gradual return to activity is recommended, following the guidance of a healthcare professional, to avoid reinjury and ensure a safe recovery process.
Preventive Measures and Risk Reduction
Prevention is key to minimizing the risk of developing tendinopathy or tendonitis. Some preventive measures include:
- Proper Warm-up and Stretching: Before the physical activity, engage in a thorough warm-up routine and perform dynamic stretches to prepare the muscles and tendons for exercise.
- Correct Training Techniques: Employ proper form and technique when engaging in sports or activities that involve repetitive movements to avoid excessive stress on the tendons.
- Adequate Rest and Recovery: Allow sufficient time for rest and recovery between activities, giving the tendons time to repair and adapt to their demands.
Conclusion
Tendinopathy and tendonitis are common conditions affecting the tendons, often resulting from overuse or acute injury. Understanding the differences between these conditions is crucial for accurate diagnosis and appropriate treatment selection. Individuals can effectively manage tendon conditions, alleviate pain, and restore optimal function by seeking early intervention, adhering to a comprehensive treatment plan, and adopting preventive measures.
If you experience tendon pain, or suspect tendinopathy or tendonitis, consult a podiatrist or sports medicine specialist. They can provide a thorough evaluation, guide you through the diagnosis process, and develop a personalized treatment plan tailored to your needs. You can overcome tendon-related challenges and regain your active lifestyle with the right approach and professional guidance.
Key Takeaways
- Tendinopathy and tendonitis are distinct conditions affecting the tendons, with tendinopathy involving degenerative changes and tendonitis characterized by inflammation.
- Accurate diagnosis is essential for effective treatment, as treatment approaches differ between tendinopathy and tendonitis.
- Early intervention, appropriate treatment modalities, and rehabilitation play crucial roles in managing tendon conditions, alleviating pain, and restoring optimal function.
FAQ
Does tendinopathy ever go away?
Tendinopathy is a chronic condition that requires proper management and care. While it may not completely go away, with appropriate treatment and rehabilitation, symptoms can be significantly reduced, allowing individuals to regain function and manage their condition effectively.
What are the three stages of tendinopathy?
Tendinopathy typically progresses through three stages:
- Reactive Stage: This initial stage involves an inflammatory response characterized by pain and localized swelling. Rest and conservative measures can often resolve symptoms at this stage.
- Tendon Dysrepair: In this stage, degenerative changes within the tendon begin to occur. The tendon may show disorganization, increased vascularity, and collagen breakdown. Treatment strategies shift towards addressing the underlying degeneration.
- Degenerative Stage: The final stage involves significant degeneration of the tendon structure. This stage may lead to tendon thickening, reduced strength, and increased risk of tendon rupture. Treatment focuses on pain management, rehabilitation, and potential surgical intervention.
When does tendinitis become tendinopathy?
Tendinitis can progress to tendinopathy when the condition becomes chronic or repeated episodes of inflammation and inadequate healing occur. Over time, the repetitive strain on the tendon can lead to degenerative changes, altering the structure and function of the tendon. Proper diagnosis and timely intervention are crucial to prevent the progression from acute tendinitis to chronic tendinopathy.

