Venous Stasis Ulcer Complications: Causes, Symptoms & Treatment
Venous stasis ulcers are a common complication of venous insufficiency and varicose veins, affecting approximately 1% of the population. These leg ulcers can be painful and debilitating, and if left untreated, they can lead to serious complications, including infections, cellulitis, and even amputation. In this article, we will discuss the causes, symptoms, and treatment of venous stasis ulcers, as well as preventive measures that can be taken to avoid this condition.
What Are Venous Stasis Ulcers?
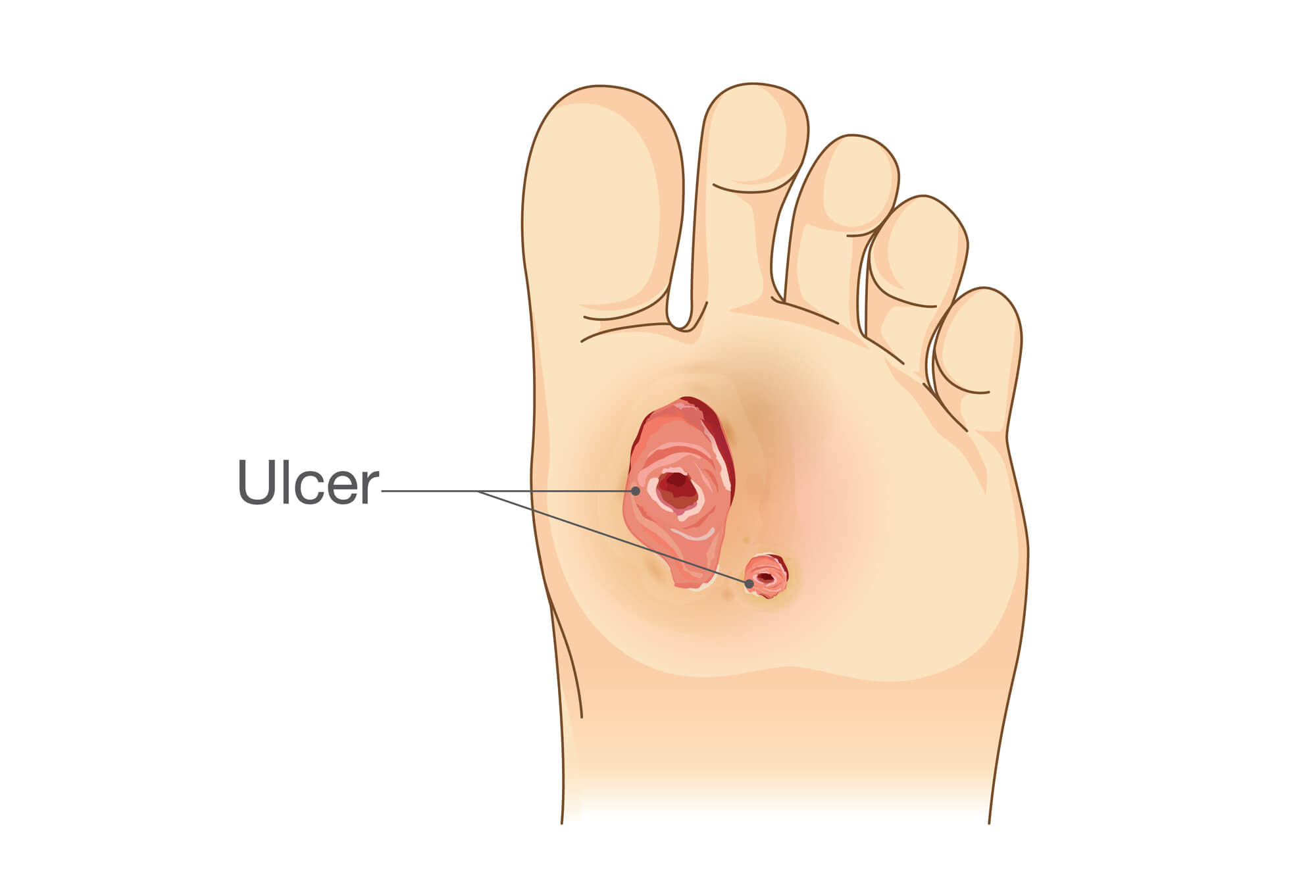
Venous stasis ulcers, or venous leg ulcers, are open sores on the lower leg due to chronic venous insufficiency. This condition occurs when the valves in the veins of the leg become damaged or weakened, leading to blood pooling in the lower leg and causing inflammation and damage to the skin and tissue.
Venous stasis ulcers are typically shallow and appear as red or purple wounds with irregular edges. Other symptoms, such as itching, burning, and pain, may accompany them.
Causes of Venous Stasis Ulcers
Venous stasis ulcers are most commonly caused by venous insufficiency and varicose veins. When the veins in the leg cannot pump blood back to the heart effectively, blood can pool in the lower leg, leading to chronic inflammation and damage to the skin and tissue. Other factors that can increase the risk of developing venous stasis ulcers include:
- Obesity
- Pregnancy
- Smoking
- Inactivity or prolonged periods of standing or sitting
- Family history of venous insufficiency or varicose veins
- Prior history of blood clots or deep vein thrombosis (DVT)
Symptoms of Venous Stasis Ulcers
The symptoms of venous stasis ulcers can vary depending on the severity of the condition. However, some common symptoms include:
- Pain and discomfort in the affected leg
- Swelling and inflammation
- Red or purple discoloration of the skin
- Itching or burning sensation
- Foul odor or drainage from the ulcer
Complications Associated with Venous Stasis Ulcers
Venous stasis ulcers can lead to a variety of complications if left untreated. These complications can include:
- Infection: The open wound of a venous stasis ulcer can be a breeding ground for bacteria, increasing the risk of infection. An infected ulcer can lead to cellulitis or even sepsis if left untreated.
- Cellulitis: Cellulitis is a bacterial infection of the skin and underlying tissue that can occur in severe venous stasis ulcers. Symptoms of cellulitis include redness, warmth, tenderness around the wound, fever, and chills.
- Deep vein thrombosis (DVT) and pulmonary embolism (PE): DVT occurs when a blood clot forms in a deep vein in the leg. If the clot breaks loose and travels to the lungs, it can cause a life-threatening pulmonary embolism.
- Chronic venous insufficiency (CVI): Chronic venous insufficiency is a long-term condition when the veins in the leg cannot pump blood back to the heart effectively. This condition can cause various symptoms, including swelling, pain, and skin changes.

Diagnosing Venous Stasis Ulcers
Diagnosing venous stasis ulcers typically involves a physical examination, medical history, and diagnostic tests such as an ultrasound or Doppler study to evaluate blood flow in the leg. Differential diagnosis may also be needed to differentiate venous stasis ulcers from other types of wounds, such as arterial or diabetic ulcers.
Treating Venous Stasis Ulcers
Treating venous stasis ulcers aims to promote wound healing and prevent complications. Treatment options include:
- Wound care and management: Keeping the wound clean and moist and applying dressings or topical treatments to promote healing. Debridement may also be necessary to remove dead tissue from the wound.
- Compression therapy: Compression stockings or bandages help improve blood flow in the leg and reduce swelling. This can help to prevent the development of new ulcers and promote the healing of existing ones.
- Medications: Antibiotics may be prescribed if an infection is present, while other medications may be used to improve blood flow and reduce inflammation.
- Surgery and other procedures: In severe cases, surgery or other procedures may be necessary to remove damaged tissue or repair damaged veins.
Preventing Venous Stasis Ulcers
Preventing venous stasis ulcers involves reducing the risk of developing chronic venous insufficiency and varicose veins. These steps include:
- Maintaining a healthy weight
- Exercising regularly
- Elevating the legs when sitting or lying down
- Avoiding prolonged periods of standing or sitting
- Wearing compression stockings if recommended by a healthcare professional
- Treating any underlying medical conditions that may increase the risk of venous insufficiency or varicose veins
Also, good hygiene practices can help prevent venous stasis ulcer complications. These include keeping the wound clean and dry, avoiding touching the wound with bare hands, and seeking medical attention promptly if any signs of infection or other complications develop.
Conclusion
Venous stasis ulcers can be a painful and debilitating, but with prompt diagnosis and treatment, most cases can be successfully managed. If you are experiencing symptoms of venous stasis ulcers or are concerned about your risk of developing this condition, it's important to speak with a healthcare professional. With the right treatment and preventive measures, you can reduce your risk of complications and improve your quality of life.

